Case Study
A Strategic Approach to Workforce Planning for the Diagnostic Imaging Workforce
Surrey and Sussex Cancer Alliance
Introduction
Surrey and Sussex Cancer Alliance (SSCA) bring together health, social care and third sector organisations to work together to transform cancer care and improve cancer survival. They work with system partners who are responsible for commissioning and providing services and lead the transformation and improvement of cancer care and services across the local health and care systems.
What was the issue/problem to address?
Surrey and Sussex Cancer Alliance recognised that there was a recruitment and retention issue in some staff groups in cancer and diagnostics services and that workforce supply and demand is challenging across their footprint.
What action was taken to address the issue?
The Alliance recognised that the need for a strategic system-wide approach to workforce planning had become imperative across the patch they cover and adopted an Optimal Workforce Planning Project. The overarching purpose was to provide recommendations for an optimal cancer workforce establishment across SSCA with the aim of reducing variation in patient experience and supporting performance improvement across the footprint. They acknowledged the need to understand the current workforce position in addition to sustaining a future workforce aligned to the needs of the population. Understanding the current workforce position was challenging as the Electronic Staff Record (ESR), the system that provides national workforce data, encompasses a variety of caveats, which resulted in the need to export establishment data from providers on an individual basis. Job descriptions and staff pay bands varied and managers described roles in different ways. The extent of variation and inconsistency informed the increased level of concern and justified the need for exploration. The need to collate accurate data to inform a true baseline position was important to enable analysis of actual gaps in comparison to perceived gaps and to determine impact following intervention.
The objectives of the workforce-planning project were to support the implementation of an optimised organisational cancer workforce structure with standardised resources including job descriptions, banding and responsibilities and to signpost career development pathways required to support succession planning. The recommendations also informed a strategic approach to proportionate funding allocation including consistent roles based on evidence of activity and workload. In addition, providing guidance to improve the effectiveness of multi-professional teams across tumour sites to optimise early diagnosis and holistic patient outcomes.
So far, SSCA have completed phase one of the project, undertaking a baseline assessment of priority cancer workforce roles across organisational structures with findings used to support the funding of additional pathway navigators to align with the Faster Diagnostic Standard and Cancer Support Workers as part of the implementation of Personalised Stratified Follow-Up. New roles are being piloted to facilitate workforce stretch aligned to the national competency frameworks for Assistant Practitioner and Advanced Clinical Practitioner levels.
The imaging Computerised Tomography (CT) example
One particular area of challenge was diagnostic imaging with an aging workforce, location/lack of appeal of sites, and a disproportionate allocation of recruits with some trusts being more successful than others. Feedback indicated that existing roles were limiting and there was a lack of career progression opportunities. In addition, access to training required flexibility and existing courses might not necessarily align to new models of operational delivery. Organisational movement was limited due to dependency on workforce stretch and growth and compromised due to historical structures.
A Sussex Imaging Transformation Workforce Reference Group, supported by Heath Education England South East (HEE SE) Workforce Transformation Team facilitated a patient pathway-mapping workshop. The group identified a shortfall in the workforce required to undertake routine, elective computerised tomography (CT) examinations and took steps to explore alternative options as a collaborative. Exploration of how the workforce establishment aligned to current and future service needs across Sussex was the vision as opposed to historical landscape was the area of focus.
The approach:
Stage one Identify key points in the pathway (pre diagnostic, during, post diagnostic)
Stage two Identify tasks and functions delivered throughout the pathway
Stage three Identify the competences required to deliver the tasks and functions and who delivers them now
Stage four Identify who could deliver the competences going forward
Stage five aligning tasks and competences to nationally recognised key functional descriptors to illustrate individual nuance and role creep.
Stage 6 aligning functional descriptors to generic role profiles with agreed understanding of purpose scope and remit
Stage 7 aligning educational content, curriculum design and method of delivery to maximise the supply and optimise the pace of transformation.
This approach illustrated the current provider workforce establishment, including a high-level baseline position across the system for transparency. Wider discussion informed standardised metrics, sharing best practice and re- mapping of the pathway in relation to actual workforce needs. The workshop approach and environment allowed the opportunity to establish a collaborative system approach with shared decision-making and an emphasis on creating cultural change.
The workshops identified the required competences at key points within the pathway and highlighted alignment to HEE functional descriptors at foundation, core, enhanced and advanced levels. The key findings included the need for a career framework across the CT pathway, the development of inter-professional role profiles aligned to functional competence and the need to extend the skills mix of the workforce. The production of a competence map with the aim to support the introduction or spread of new roles across the diagnostics workforce illustrated a process to increase skill mix, support upskilling, and promote consistency of roles and consistent job descriptions. Further workshops to explore a cohort approach to accessing accredited programmes of education and training embedding a variety of delivery options including apprenticeships, upskilling and return to practice will further inform sustainable recommendations.
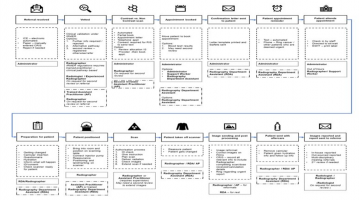
The competences for the Computerised Tomography (CT) pathway are set out below:
Key observations included missed opportunity to embed the Assistant Practitioner as a practitioner working autonomously within the scope of set protocols. Workshop attendees agreed that the role has potential added value with particular reference to workforce growth and may take steps towards addressing the surplus in demand for routine imaging by increasing capacity, for example Community Diagnostic Centres.
Further recommendations include the need to explore and develop the role of the Radiography Department Assistant as a foundation level entry point. Current workforce planning trajectories suggest that the shortfall in supply of registered staff continues to grow with establishment needs calculated using historical workforce structures. It takes between three to five years to complete the required level of education, training, and competence providing eligibility to apply for registration with the Health Care Professions Council (HCPC). Registration allows candidates to work autonomously, with statutory responsibility within the legal scope and remit of radiation regulation. Responsibility for safe practice remains with the registered workforce; however, the opportunity to delegate authority aligned to evidence of competency is apparent. Opportunity to utilise competent workforce groups to deliver routine imaging examinations aligned to specific protocol was identified as a priority for workforce redesign. Furthermore, suggestion that non-contrast scans currently undertaken by Band 5/6 radiographers undertaken by a Foundation Practitioner who has completed appropriate education, training and competences may take steps towards closing the workforce shortfall. This approach provides a springboard for valued members of the workforce to enter a sustainable career development pathway embedding principles of widening participation. Utilising current provision of accredited programmes of education such as the Undergraduate Certificate in Imaging and Diploma of Higher Education adopts a true workforce transformation process facilitating a reduction in the shortfall of workforce establishment as a long term strategic approach.
What difficulties and barriers needed to be overcome to implement the change?
The ability to provide clear career progression pathways that are agile and responsive to current and future workforce profiles is challenging and unable to be progressed at pace. There were some difficulties and barriers including a lack of understanding about what funding was available to facilitate transformation and upskilling. The challenge of embracing organisational change will require a cultural shift. This approach (like all workforce planning) is time-consuming with operational priorities taking precedence. Providers have committed to attending and participating in the workshops and have wanted to explore alternative solutions actively, with a focus on transferable skills and competences, rather than who delivered them. Emphasis was applied to identifying and agreeing key principles that can be applied across services and geographical boundaries.
What benefits have resulted from the change?
By extending the skills mix of the workforce across the CT pathway, tasks and functions can be delivered by members of the workforce with the appropriate competences aligned to service and patient needs. This could result in the time of radiographers being released to lead and supervise their teams. It will also enable radiographers to focus upon the tasks and functions that are statutory to registered personnel and undertake career development and progression activities, and programmes of study to meet the gap in supply at advanced practice level. It will enable practitioners to work at the top of their licence and provide career opportunities across the different roles and the development of new roles such as the Foundation and Assistant Practitioner roles. The approach aligns workforce establishments to embed sustainable initiatives such as the South East Imaging Academy framework and maximise the impact of funding opportunities to address workforce needs.
What tips can you pass on to other organisation’s and NHS employers?
SSCA recognise that the Optimal Workforce Planning Project approach will evolve and will be transferable to multiple workforce groups and service redesign. There is now a need to share and discuss findings with providers, share best practice, agree standardised responsibilities, role profiles, and job descriptions. Alignment to regional and national recommendations is imperative to enable true workforce stretch, growth and sustainability.
Megan Wilkins Workforce and Education Manager with Surrey and Sussex Alliance says:
‘’ Initially there was resistance to this approach to workforce planning, but there was engagement from staff when they understood the methodology as there is a recognition that the recruitment and retention of radiographers is a huge challenge in the South East. By undertaking this approach system-wide gave the process more credibility. We intend to use this approach with other service areas in the cancer and diagnostics pathway’’
Contact Megan Wilkins, Workforce and Education Manager megan.wilkins2@nhs.net